Volunteer
Use this page to list volunteer opportunities and current job openings. Donec ultrices ex ut ante consectetur, sed varius libero pharetra. Aenean consequat orci metus, in tempus erat venenatis sed. Donec ut est et tortor rhoncus aliquet. Nulla sollicitudin, sapien quis malesuada semper, felis lectus eleifend ipsum, ultrices hendrerit turpis lorem sit amet nunc. Aenean facilisis leo sapien, eget congue justo sollicitudin at. Morbi a elit at mi pulvinar vulputate. Etiam bibendum sed lorem ut mollis.

“
October 2017
This is an example testimonial. Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed nec vestibulum augue. Sed purus felis, sollicitudin vel arcu sit amet.
Quote Source / Read Full Article
“
Septemer 2017
This is an example testimonial. Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed nec vestibulum augue. Sed purus felis, sollicitudin vel arcu sit amet.
Quote Source / Read Full Article
“
August 2017
This is an example testimonial. Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed nec vestibulum augue. Sed purus felis, sollicitudin vel arcu sit amet.
Quote Source / Read Full Article
“
July 2017
This is an example testimonial. Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed nec vestibulum augue. Sed purus felis, sollicitudin vel arcu sit amet.
Quote Source / Read Full Article
“
June 2017
This is an example testimonial. Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed nec vestibulum augue. Sed purus felis, sollicitudin vel arcu sit amet.
Quote Source / Read Full Article
“
May 2017
This is an example testimonial. Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed nec vestibulum augue. Sed purus felis, sollicitudin vel arcu sit amet.
Quote Source / Read Full Article
Our Partners
Partner 1
Here is a description of a partner organization. Integer euismod, lorem sed molestie gravida, justo mauris dignissim orci, sed convallis elit at justo. Donec feugiat justo vitae mollis pretium.
Partner 2
Here is a description of a partner organization. Integer euismod, lorem sed molestie gravida, justo mauris dignissim orci, sed convallis elit at justo. Donec feugiat justo vitae mollis pretium.
Partner 3
Here is a description of a partner organization. Integer euismod, lorem sed molestie gravida, justo mauris dignissim orci, sed convallis elit at justo. Donec feugiat justo vitae mollis pretium.
Partner 4
Here is a description of a partner organization. Integer euismod, lorem sed molestie gravida, justo mauris dignissim orci, sed convallis elit at justo. Donec feugiat justo vitae mollis pretium.
Partner 5
Here is a description of a partner organization. Integer euismod, lorem sed molestie gravida, justo mauris dignissim orci, sed convallis elit at justo. Donec feugiat justo vitae mollis pretium.
Partner 6
Here is a description of a partner organization. Integer euismod, lorem sed molestie gravida, justo mauris dignissim orci, sed convallis elit at justo. Donec feugiat justo vitae mollis pretium.
Partner 7
Here is a description of a partner organization. Integer euismod, lorem sed molestie gravida, justo mauris dignissim orci, sed convallis elit at justo. Donec feugiat justo vitae mollis pretium.
Partner 8
Here is a description of a partner organization. Integer euismod, lorem sed molestie gravida, justo mauris dignissim orci, sed convallis elit at justo. Donec feugiat justo vitae mollis pretium.
Our Programs
Example Program 1
Here is a description of your program. Quam tempus quis. Nullam luctus elit quis blandit elementum. Nulla quis nisi nec dolor facilisis cursus. Donec dictum et orci ac varius. Nam sed arcu ligula. Suspendisse at purus ut velit gravida malesuada eu a ipsum. Quisque eget nisl fringilla, lacinia lorem id, malesuada ante. Sed dignissim diam a quam ultrices sodales. Suspendisse consectetur velit purus, eget lobortis erat varius sed.
Donec ultrices ex ut ante consectetur, sed varius libero pharetra. Aenean consequat orci metus, in tempus erat venenatis sed. Donec ut est et tortor rhoncus aliquet. Nulla sollicitudin, sapien quis malesuada semper, felis lectus eleifend ipsum, ultrices hendrerit turpis lorem sit amet nunc. Aenean facilisis leo sapien, eget congue justo sollicitudin at. Morbi a elit at mi pulvinar vulputate. Etiam bibendum sed lorem ut mollis.
Availability
Monday – Saturday
Morning, Afternoon or Evening
Location
123 Demo Street
Manhattan, NY 12345
Example Program 2
Here is a description of your program. Quam tempus quis. Nullam luctus elit quis blandit elementum. Nulla quis nisi nec dolor facilisis cursus. Donec dictum et orci ac varius. Nam sed arcu ligula. Suspendisse at purus ut velit gravida malesuada eu a ipsum. Quisque eget nisl fringilla, lacinia lorem id, malesuada ante. Sed dignissim diam a quam ultrices sodales. Suspendisse consectetur velit purus, eget lobortis erat varius sed.
Donec ultrices ex ut ante consectetur, sed varius libero pharetra. Aenean consequat orci metus, in tempus erat venenatis sed. Donec ut est et tortor rhoncus aliquet. Nulla sollicitudin, sapien quis malesuada semper, felis lectus eleifend ipsum, ultrices hendrerit turpis lorem sit amet nunc. Aenean facilisis leo sapien, eget congue justo sollicitudin at. Morbi a elit at mi pulvinar vulputate. Etiam bibendum sed lorem ut mollis.
Availability
Monday – Saturday
Morning, Afternoon or Evening
Location
123 Demo Street
Manhattan, NY 12345
Example Program 3
Here is a description of your program. quam tempus quis. Nullam luctus elit quis blandit elementum. Nulla quis nisi nec dolor facilisis cursus. Donec dictum et orci ac varius. Nam sed arcu ligula. Suspendisse at purus ut velit gravida malesuada eu a ipsum. Quisque eget nisl fringilla, lacinia lorem id, malesuada ante. Sed dignissim diam a quam ultrices sodales. Suspendisse consectetur velit purus, eget lobortis erat varius sed.
Donec ultrices ex ut ante consectetur, sed varius libero pharetra. Aenean consequat orci metus, in tempus erat venenatis sed. Donec ut est et tortor rhoncus aliquet. Nulla sollicitudin, sapien quis malesuada semper, felis lectus eleifend ipsum, ultrices hendrerit turpis lorem sit amet nunc. Aenean facilisis leo sapien, eget congue justo sollicitudin at. Morbi a elit at mi pulvinar vulputate. Etiam bibendum sed lorem ut mollis.
Availability
Monday – Saturday
Morning, Afternoon or Evening
Location
123 Demo Street
Manhattan, NY 12345
Example Program 4
Here is a description of your program. Quam tempus quis. Nullam luctus elit quis blandit elementum. Nulla quis nisi nec dolor facilisis cursus. Donec dictum et orci ac varius. Nam sed arcu ligula. Suspendisse at purus ut velit gravida malesuada eu a ipsum. Quisque eget nisl fringilla, lacinia lorem id, malesuada ante. Sed dignissim diam a quam ultrices sodales. Suspendisse consectetur velit purus, eget lobortis erat varius sed.
Donec ultrices ex ut ante consectetur, sed varius libero pharetra. Aenean consequat orci metus, in tempus erat venenatis sed. Donec ut est et tortor rhoncus aliquet. Nulla sollicitudin, sapien quis malesuada semper, felis lectus eleifend ipsum, ultrices hendrerit turpis lorem sit amet nunc. Aenean facilisis leo sapien, eget congue justo sollicitudin at. Morbi a elit at mi pulvinar vulputate. Etiam bibendum sed lorem ut mollis.
Availability
Monday – Saturday
Morning, Afternoon or Evening
Location
123 Demo Street
Manhattan, NY 12345
Example Program 5
Here is a description of your program. Quam tempus quis. Nullam luctus elit quis blandit elementum. Nulla quis nisi nec dolor facilisis cursus. Donec dictum et orci ac varius. Nam sed arcu ligula. Suspendisse at purus ut velit gravida malesuada eu a ipsum. Quisque eget nisl fringilla, lacinia lorem id, malesuada ante. Sed dignissim diam a quam ultrices sodales. Suspendisse consectetur velit purus, eget lobortis erat varius sed.
Donec ultrices ex ut ante consectetur, sed varius libero pharetra. Aenean consequat orci metus, in tempus erat venenatis sed. Donec ut est et tortor rhoncus aliquet. Nulla sollicitudin, sapien quis malesuada semper, felis lectus eleifend ipsum, ultrices hendrerit turpis lorem sit amet nunc. Aenean facilisis leo sapien, eget congue justo sollicitudin at. Morbi a elit at mi pulvinar vulputate. Etiam bibendum sed lorem ut mollis.
Availability
Monday – Saturday
Morning, Afternoon or Evening
Location
123 Demo Street
Manhattan, NY 12345
Example Program 6
Here is a description of your program. Quam tempus quis. Nullam luctus elit quis blandit elementum. Nulla quis nisi nec dolor facilisis cursus. Donec dictum et orci ac varius. Nam sed arcu ligula. Suspendisse at purus ut velit gravida malesuada eu a ipsum. Quisque eget nisl fringilla, lacinia lorem id, malesuada ante. Sed dignissim diam a quam ultrices sodales. Suspendisse consectetur velit purus, eget lobortis erat varius sed.
Donec ultrices ex ut ante consectetur, sed varius libero pharetra. Aenean consequat orci metus, in tempus erat venenatis sed. Donec ut est et tortor rhoncus aliquet. Nulla sollicitudin, sapien quis malesuada semper, felis lectus eleifend ipsum, ultrices hendrerit turpis lorem sit amet nunc. Aenean facilisis leo sapien, eget congue justo sollicitudin at. Morbi a elit at mi pulvinar vulputate. Etiam bibendum sed lorem ut mollis.
Availability
Monday – Saturday
Morning, Afternoon or Evening
Location
123 Demo Street
Manhattan, NY 12345
Our Impact
Use this page to describe the accomplishments of your organization or company. Lorem ipsum dolor sit amet, consectetur adipiscing elit. Mauris et leo et ante vestibulum tristique ut quis lacus. Fusce ut sem ac tortor imperdiet finibus. Maecenas semper urna sit amet arcu egestas, et condimentum urna fermentum. Aliquam euismod turpis at mauris condimentum, vitae vestibulum erat fermentum. Pellentesque nec mattis nunc. Suspendisse tincidunt eros sed dignissim dapibus. Maecenas rutrum leo at lacinia pulvinar.
Pellentesque vitae nisl quis ante accumsan cursus eleifend sit amet leo. Duis nisi nibh, porttitor eu felis auctor, sollicitudin viverra mi. Aliquam non nulla vitae nisl pretium auctor ac et urna. Proin quis neque libero. Nam vestibulum, lorem nec molestie ultricies, mauris sem luctus dolor, a facilisis lectus urna nec nisi. Nam malesuada, neque posuere maximus sollicitudin, felis eros vulputate dui, a efficitur lacus massa sed enim. Nullam arcu arcu, malesuada vitae lorem et, vestibulum faucibus dolor. Fusce quis arcu eget tellus vestibulum tristique. Fusce vel nisl tortor. Donec rhoncus mi orci, luctus fringilla urna mattis vitae.
Aenean blandit, lectus sed tempor egestas, dui nisi dictum arcu, quis efficitur nulla lectus congue eros. Vivamus volutpat eget neque ut feugiat. Pellentesque pharetra velit sit amet nibh placerat, non feugiat mi laoreet. Sed enim ex, imperdiet cursus est id, venenatis dictum nulla. Nullam pulvinar lacus nec nibh efficitur, vitae aliquet orci accumsan. Nunc at erat vitae enim viverra congue. Ut luctus dolor elit, a euismod sem euismod nec. Mauris id libero ligula. Donec mollis at sem id tincidunt. Nunc vel malesuada ipsum. Mauris gravida, sapien vel porta commodo, eros arcu faucibus metus, ac iaculis felis lectus in est. Fusce diam magna, ullamcorper nec maximus sit amet, euismod non metus. Nullam dolor elit, aliquet non nisl eget, ultricies placerat ex. Nunc egestas viverra mauris id tristique. Donec ex lacus, scelerisque et nulla at, fringilla porttitor nisi. Ut nec nibh ac justo congue sollicitudin.
Fusce faucibus venenatis dui, quis ornare nisl gravida eu. Curabitur facilisis posuere tempus. Donec in erat eu arcu elementum ornare eu vitae tellus. Nunc lectus lorem, gravida quis massa et, venenatis pulvinar felis. Sed maximus eget velit ut blandit. Morbi luctus tortor et lectus lobortis, a dapibus velit placerat. Vivamus fringilla ante ut cursus ullamcorper. Pellentesque laoreet sagittis posuere.
Praesent vel diam ut arcu tempus eleifend at id leo. Nullam eget felis aliquet, consequat nibh quis, luctus tortor. Aliquam a dolor euismod mi congue tempus quis eu magna. Ut vestibulum sapien urna, elementum maximus lacus condimentum nec. Donec purus urna, rutrum et erat sed, feugiat rutrum risus. Curabitur luctus maximus condimentum. Duis blandit ligula vitae erat sodales, eu molestie mi placerat. Morbi vulputate velit et placerat hendrerit. Praesent sollicitudin augue urna, non ultrices sapien cursus ut. Donec id justo vel metus sollicitudin hendrerit. Nullam fermentum finibus dignissim.
EDI 101
1. EDI & X12 Essentials: Navigating Data Exchange in Healthcare
EDI is the file format used in submitting Risk Adjustment Encounter Data to CMS. Electronic Data Interchange (EDI), with the X12 standard is the most widely adopted format in the U.S. for healthcare transactions.
This guide breaks down the essentials of EDI and X12, their structural components, and how they support crucial workflows in healthcare claim submissions and responses.
🔹 What is EDI?
Electronic Data Interchange (EDI) allows different organizations to electronically exchange data using standardized formats. In healthcare, this means replacing paper-based processes with automated digital messages—for example, sending a claim from a provider to a payer system.
With EDI, tasks like submitting claims, receiving payment remittance, checking eligibility, and requesting prior authorizations become faster, more accurate, and scalable.
🔹 Introduction to X12
The X12 standard, maintained by the Accredited Standards Committee (ASC) X12, defines specific formats for EDI transactions. Here’s a simplified list of commonly used EDI files in healthcare and what they’re used for:
837 – Healthcare Claim (Professional, Institutional, Dental):
Used by providers to submit claim data to payers.TA1 – Interchange Acknowledgment:
Confirms the EDI file was received and checks for format or envelope-level errors (e.g., ISA/GS errors).999 – Implementation Acknowledgment:
Indicates whether the file passes syntactic and structural checks. Notifies of issues at the transaction set level.277CA – Claim Acknowledgment:
Indicates whether individual claims in an accepted file were accepted, rejected, or pended at the business level.
Each file format follows a strict structure, ensuring reliable automation and interoperability across systems.
🔹 The X12 Document Hierarchy
X12 files are organized in a nested structure, much like Russian dolls:
Envelope Level:
ISA (start) and IEA (end) define the interchange
GS/GE pair defines functional groups (e.g., all professional claims)
ST/SE pairs contain individual transaction sets (e.g., one claim submission)
Loops: Each loop defines a logical block (e.g., patient info, provider info).
Segments: Segments are lines beginning with identifiers like NM1, REF, DTP.
Elements: Elements are data fields within a segment, separated by asterisks *.
Sub-elements: Occasionally, elements are further split using colons :.
Example Segment:
NM1*41*2*Health Payer System*****46*TGJ23~
This can be broken down to mean the billing service (entity code 41) submitting the claim.
🔹 Understanding Key Segments & Loops
NM1 (Name Segment): Provides the name or identifier of an entity (e.g., provider, patient).
REF (Reference Identifier): Adds extra identification (e.g., internal control numbers).
DTP (Date or Time Period): Indicates service dates.
Common Loops in an 837 File:
Loop Purpose
1000A Submitter (billing provider or clearinghouse)
1000B Receiver (payer)
2000A Billing provider hierarchy
2000B Subscriber/patient information
2300 Claim information
2400 Service line details
🔹 Sample Flow: From Claim to Payment
837 is submitted by the provider.
TA1 acknowledges formatting at envelope level.
999 acknowledges syntax/structure.
277CA confirms claim was accepted (or rejected) by payer.
Each step helps track and validate the lifecycle of a claim, ensuring accountability and reducing payment delays.
🔹 Visualizing the Claim Processing Lifecycle
A conceptual flow diagram typically accompanies this section showing the transition from 837 → TA1 → 999 → 277CA
🔹 Key Takeaways for Healthcare Teams
Adopting EDI/X12 formats reduces manual intervention, enhances data accuracy, and speeds up reimbursement cycles.
Understanding loop/segment structure is critical for troubleshooting rejections and interpreting remittance files.
Files like 999 and 277CA provide early insights into issues that might delay payment.
📚 Additional Resources
Internal: 837P Companion Guide
Knowledge Base: Annotated 837 Dental Claim Explainer
If you're part of a provider organization or payer working with Medicare Advantage or commercial plans, EDI compliance and literacy is more than a technical necessity—it's a financial imperative. Mastering these formats ensures cleaner submissions, fewer rejections, and faster payments.
2. Understanding EDI Acknowledgment Files: A Guide to 999 and 277CA Responses
Electronic Data Interchange (EDI) is at the heart of modern healthcare claim submissions, particularly in the Medicare Advantage and Medicaid environments. Two crucial types of acknowledgment files—EDI 999 Functional Acknowledgment and EDI 277 Claim Acknowledgment (277CA)—serve as feedback mechanisms from the payer or clearinghouse, informing healthcare providers and submitters about the status and acceptance of their claims. This blog unpacks the essentials of these acknowledgment reports, helping you better interpret and resolve errors for cleaner, faster claims processing.
🔹 What Is the EDI 999 Functional Acknowledgment?
The 999 file confirms whether an EDI file, such as an 837 claim transaction, was accepted or rejected at the syntax level. It is generated by the receiver system (payer or clearinghouse) to let you know whether the EDI file was structurally correct.
Key Segments in 999:
Segment Purpose
ISA/GS Envelope Headers
AK1 Functional Group Acknowledgment
AK2 Transaction Set Acknowledgment
IK3 Identifies the segment containing the error
IK4 Pinpoints the element or component with the error
IK5 Final status of the transaction set
IK5 Acknowledgment Codes:
Code Description
A Accepted
E Accepted with errors
R Rejected
P Partially accepted
W Rejected due to warnings
Examples of Common Errors:
Segment Error Description
ISA Invalid sender or receiver ID
GS Functional group mismatch
NM1 Missing or invalid provider information
REF Misused reference qualifiers
CLM Claim data invalid or formatted wrongly
✅ Pro Tip: A rejected 999 means your file didn’t even make it to claim processing. Resolve these errors immediately to avoid delays.
🔹 What Is the EDI 277 Claim Acknowledgment (277CA)?
The 277CA file tracks the status of each individual claim within a submitted batch once it passes the syntax check (i.e., after a successful 999). It provides detailed updates on whether the claim was accepted into the adjudication system, pended, rejected, or finalized.
Key Segments in 277CA:
Segment Purpose
BHT Beginning of Hierarchical Transaction
TRN Claim Trace Number
STC Claim Status Category Code
DTP Date and time the status was updated
REF Additional identifiers (e.g., Payer Claim Number)
STC Claim Status Codes:
Code Meaning
A1 Acknowledged
A2 Acknowledged with errors
A3 Rejected
P0 In process
F1 Finalized – Paid
F2 Finalized – Denied
Common Error Category Codes in STC:
Code Description
15 Required information missing
21 Invalid or missing provider number
22 Invalid or missing patient ID
23 Claim filing indicator missing
42 Duplicate claim
85 Rendering provider not enrolled
187 Invalid diagnosis code
🔍 Insight: A “P0” status may seem reassuring, but continued "pending" claims may indicate systemic issues that need resolution.
🛠 Why These Acknowledgments Matter
Compliance Assurance: A successful 999 and 277CA flow ensures your organization adheres to HIPAA-mandated EDI standards.
Faster Reimbursements: Catching and correcting syntax and structural issues early accelerates claim approval.
Root Cause Analysis: Frequent rejections (e.g., due to NM1 or CLM errors) can reveal training or system configuration gaps in your RCM workflow.
✅ Best Practices
Automate parsing of 999/277 files within your RCM platform to alert billing teams in real time.
Track IK3 and IK4 patterns to identify recurring formatting issues.
Use dashboards to visualize rejection reasons over time and by payer.
Map TRN references back to original claim IDs for faster troubleshooting.
Ensure clean provider and patient data upfront to minimize rejections tied to STC codes like 21, 22, or 85.
Final Thoughts
Navigating the 999 and 277CA acknowledgments can seem daunting, but they offer invaluable insight into how your claims are being received and processed. Mastering these files reduces denials, shortens revenue cycles, and ensures a smoother path to payment.
Whether you're a health plan, billing vendor, or provider group, having a streamlined EDI response handling process isn't just a technical requirement—it’s a strategic advantage.
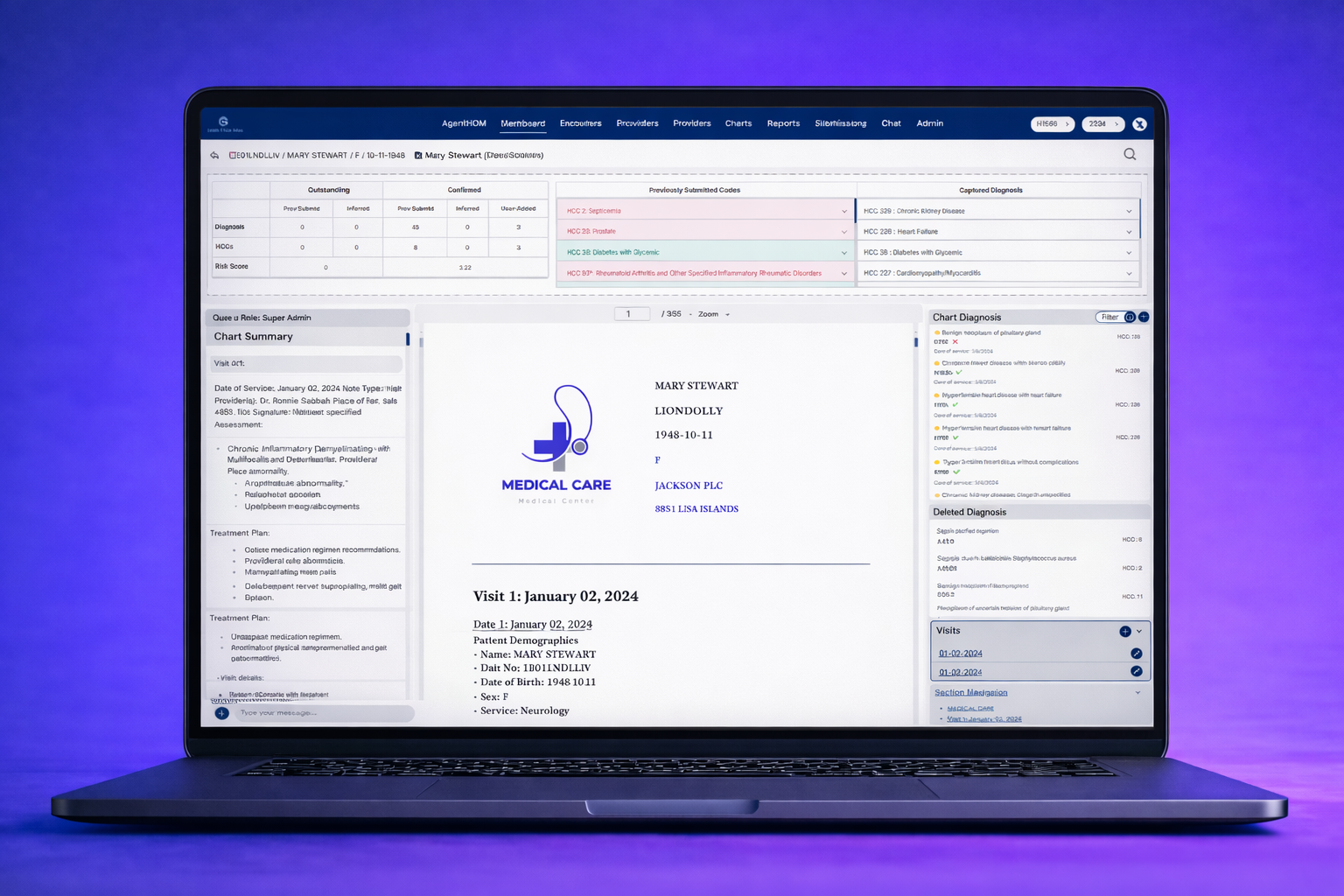
ChartCopilot™ Retro
AI-Powered Retrospective Chart Coding for Risk Adjustment and RADV Compliance
“Transform Your Retrospective Chart Coding with AI Copilots”
Agentic AI Chart Review Intelligence
ChartCopilot™ leverages Agentic AI reviewers—autonomous agents that read and interpret provider notes, lab results, and discharge summaries using fine-tuned clinical LLMs. Each agent evaluates whether documentation meets CMS’s MEAT criteria (Monitor, Evaluate, Assess, Treat), flags ambiguous evidence, and recommends clarifications for documentation improvement.
This multi-agent review system mimics the reasoning of experienced auditors, ensuring every captured diagnosis is supported, defensible, and fully RADV-ready.
Why ChartCopilot™ Retro?
Retrospective chart review is complex and time sensitive. HDM ChartCopilot™ Retro leverages fine-tuned large language models (LLMs) to accelerate chart abstraction, improve coding accuracy, and provide audit-ready documentation. Our solution combines human expertise with AI guidance to ensure:
Accurate HCC and risk score validation
Faster chart review cycles and reduced administrative burden
Ready-to-submit RADV packets with confidence
Integrated audit trails for CMS and internal compliance
Key Differentiators:
AI Coder Copilot: Guides your coders with real-time suggestions, flagging potential HCCs, documentation gaps, and MEAT compliance.
Smart Chart Navigation: Jump to relevant labs, progress notes, or visit summaries instantly with AI-assisted search.
Audit-Ready Workflows: Build RADV packets, track IRR and QA, and generate reports for internal or CMS audits.
Actionable Analytics: Visualize coding patterns, chart quality, and risk score trends to drive targeted improvements.
Compliance & Security: HIPAA-compliant, secure environment with granular access control and audit logs.
Who Should Use This?
HDM ChartCopilot™ Retro is ideal for:
Medicare Advantage Plans & Risk Adjustment Teams: Accelerate retrospective coding and ensure compliance.
Coding & QA Specialists: Reduce manual effort while improving accuracy.
Consultants & Audit Teams: Generate RADV-ready packets efficiently.
Executives & Managers: Gain visibility into risk adjustment performance and team productivity.
How It Works
Step 1: Upload & Integrate
Seamlessly import charts from EMRs, claim systems, or structured data sources. Our secure platform ensures data integrity at every step.
Step 2: AI-Assisted Coding
LLM-powered copilots provide:
Suggested HCC codes based on chart content
Real-time MEAT/TAMPER compliance checks
Highlights of missing or inconsistent documentation
Step 3: Evidence Linking
Automatically link charts, notes, and labs to each suggested HCC. The AI identifies supporting evidence and flags discrepancies.
Step 4: QA & IRR Checks
Track inter-rater reliability, coder performance, and quality assurance metrics with an intuitive dashboard.
Step 5: RADV Packet Builder
Generate fully compliant retrospective chart packets with all supporting documentation ready for submission to CMS or internal audit.
Step 6: Analytics & Insights
Measure coding efficiency, identify high-risk gaps, track coder trends, and evaluate population-level risk scoring accuracy.
Features at a Glance
LLM Coder Copilot - Suggests HCCs, highlights documentation gaps, and accelerates coder decision-making.
Smart Navigation - Jump between charts, labs, and visit notes instantly.
Evidence Linking - Automatically link supporting documents to HCCs.
IRR / QA Dashboard - Track coding accuracy, inter-rater reliability, and QA metrics.
RADV Packet Builder - Export CMS-ready retrospective packets with full audit trails.
Analytics & Insights - Monitor coding patterns, risk score trends, and chart quality.
Customizable Workflows - Configure tasks, review sequences, and alerts to match your processes.
Secure & HIPAA-Compliant - End-to-end encryption and role-based access control.
Integration-Ready - Works with EMRs, EHRs, and existing risk adjustment systems.
Expanded Benefits & Outcomes
Improve Coding Accuracy: Reduce missed HCCs and improve risk score reliability.
Boost Productivity: AI-assisted coding reduces chart review time by up to 50%, freeing staff for high-value tasks.
Streamline Audit Preparation: RADV-ready packets simplify internal and CMS audits.
Gain Visibility: Track performance across coders, departments, and facilities.
Enhance Decision-Making: Analytics identify trends, gaps, and opportunities to optimize risk adjustment performance.
Reduce Compliance Risk: AI copilot flags missing documentation, MEAT inconsistencies, and HCC discrepancies.
Integrated With Your Workflow
HDM ChartCopilot™ Retro works alongside your existing systems:
EMRs & EHRs (Epic, Cerner, Allscripts, etc.)
Risk adjustment and revenue cycle management tools
Reporting and analytics platforms
Benefit: Minimal disruption to current operations—your team can adopt AI-assisted retrospective chart coding immediately.
Security & Compliance
HIPAA-compliant data handling and secure cloud infrastructure
Detailed audit trails for every coder action
Granular role-based access controls
On-premises deployment option for organizations with internal IT requirements
Enhanced User Experience
Intuitive Interface: Simple, clean dashboards for coders and managers
Adaptive AI Assistance: Suggestions improve over time based on coder decisions
Collaborative Coding: Coders can leave notes, share findings, and resolve queries efficiently
Mobile & Remote Access: Secure access from any location for distributed teams
Client Success Stories
"With HDM ChartCopilot™ Retro, we reduced chart review time by 40% and improved coding accuracy. Preparing RADV packets has never been easier."
— Medicare Advantage Plan Risk Adjustment Director
"The AI copilot flags missing documentation and guides coders in real time, saving countless hours."
— Senior Coding Auditor
"Analytics dashboards give us actionable insights into risk score gaps across multiple facilities."
— Health Plan Executive
FAQs
Q: Can HDM ChartCopilot™ Retro integrate with my EMR?
A: Yes, our solution supports most EMRs and claim systems, allowing direct chart imports.
Q: Is the AI making final coding decisions?
A: No, the AI assists your coders by highlighting potential HCCs and documentation, but final coding remains under human review.
Q: How secure is my data?
A: HDM ChartCopilot™ Retro is fully HIPAA-compliant, with end-to-end encryption and audit logs for all actions.
Q: How quickly can we see ROI?
A: Most clients report measurable productivity gains and coding accuracy improvements within the first 60 days of deployment.
Q: Can we customize workflows?
A: Yes, you can configure task sequences, alerts, and review processes to match your organizational needs.
Get Started Today
Accelerate retrospective chart coding, improve risk adjustment accuracy, and prepare RADV-ready charts efficiently.
ChartCopilot™ Retro
AI-Powered Retrospective Chart Coding for Risk Adjustment and RADV Compliance
“Transform Your Retrospective Chart Coding with AI Copilots”
Agentic AI Chart Review Intelligence
ChartCopilot™ leverages Agentic AI reviewers—autonomous agents that read and interpret provider notes, lab results, and discharge summaries using fine-tuned clinical LLMs. Each agent evaluates whether documentation meets CMS’s MEAT criteria (Monitor, Evaluate, Assess, Treat), flags ambiguous evidence, and recommends clarifications for documentation improvement.
This multi-agent review system mimics the reasoning of experienced auditors, ensuring every captured diagnosis is supported, defensible, and fully RADV-ready.
Why ChartCopilot™ Retro?
Retrospective chart review is complex and time sensitive. HDM ChartCopilot™ Retro leverages fine-tuned large language models (LLMs) to accelerate chart abstraction, improve coding accuracy, and provide audit-ready documentation. Our solution combines human expertise with AI guidance to ensure:
Accurate HCC and risk score validation
Faster chart review cycles and reduced administrative burden
Ready-to-submit RADV packets with confidence
Integrated audit trails for CMS and internal compliance
Key Differentiators:
AI Coder Copilot: Guides your coders with real-time suggestions, flagging potential HCCs, documentation gaps, and MEAT compliance.
Smart Chart Navigation: Jump to relevant labs, progress notes, or visit summaries instantly with AI-assisted search.
Audit-Ready Workflows: Build RADV packets, track IRR and QA, and generate reports for internal or CMS audits.
Actionable Analytics: Visualize coding patterns, chart quality, and risk score trends to drive targeted improvements.
Compliance & Security: HIPAA-compliant, secure environment with granular access control and audit logs.
Who Should Use This?
HDM ChartCopilot™ Retro is ideal for:
Medicare Advantage Plans & Risk Adjustment Teams: Accelerate retrospective coding and ensure compliance.
Coding & QA Specialists: Reduce manual effort while improving accuracy.
Consultants & Audit Teams: Generate RADV-ready packets efficiently.
Executives & Managers: Gain visibility into risk adjustment performance and team productivity.
How It Works
Step 1: Upload & Integrate
Seamlessly import charts from EMRs, claim systems, or structured data sources. Our secure platform ensures data integrity at every step.
Step 2: AI-Assisted Coding
LLM-powered copilots provide:
Suggested HCC codes based on chart content
Real-time MEAT/TAMPER compliance checks
Highlights of missing or inconsistent documentation
Step 3: Evidence Linking
Automatically link charts, notes, and labs to each suggested HCC. The AI identifies supporting evidence and flags discrepancies.
Step 4: QA & IRR Checks
Track inter-rater reliability, coder performance, and quality assurance metrics with an intuitive dashboard.
Step 5: RADV Packet Builder
Generate fully compliant retrospective chart packets with all supporting documentation ready for submission to CMS or internal audit.
Step 6: Analytics & Insights
Measure coding efficiency, identify high-risk gaps, track coder trends, and evaluate population-level risk scoring accuracy.
Features at a Glance
LLM Coder Copilot - Suggests HCCs, highlights documentation gaps, and accelerates coder decision-making.
Smart Navigation - Jump between charts, labs, and visit notes instantly.
Evidence Linking - Automatically link supporting documents to HCCs.
IRR / QA Dashboard - Track coding accuracy, inter-rater reliability, and QA metrics.
RADV Packet Builder - Export CMS-ready retrospective packets with full audit trails.
Analytics & Insights - Monitor coding patterns, risk score trends, and chart quality.
Customizable Workflows - Configure tasks, review sequences, and alerts to match your processes.
Secure & HIPAA-Compliant - End-to-end encryption and role-based access control.
Integration-Ready - Works with EMRs, EHRs, and existing risk adjustment systems.
Expanded Benefits & Outcomes
Improve Coding Accuracy: Reduce missed HCCs and improve risk score reliability.
Boost Productivity: AI-assisted coding reduces chart review time by up to 50%, freeing staff for high-value tasks.
Streamline Audit Preparation: RADV-ready packets simplify internal and CMS audits.
Gain Visibility: Track performance across coders, departments, and facilities.
Enhance Decision-Making: Analytics identify trends, gaps, and opportunities to optimize risk adjustment performance.
Reduce Compliance Risk: AI copilot flags missing documentation, MEAT inconsistencies, and HCC discrepancies.
Integrated With Your Workflow
HDM ChartCopilot™ Retro works alongside your existing systems:
EMRs & EHRs (Epic, Cerner, Allscripts, etc.)
Risk adjustment and revenue cycle management tools
Reporting and analytics platforms
Benefit: Minimal disruption to current operations—your team can adopt AI-assisted retrospective chart coding immediately.
Security & Compliance
HIPAA-compliant data handling and secure cloud infrastructure
Detailed audit trails for every coder action
Granular role-based access controls
On-premises deployment option for organizations with internal IT requirements
Enhanced User Experience
Intuitive Interface: Simple, clean dashboards for coders and managers
Adaptive AI Assistance: Suggestions improve over time based on coder decisions
Collaborative Coding: Coders can leave notes, share findings, and resolve queries efficiently
Mobile & Remote Access: Secure access from any location for distributed teams
Client Success Stories
"With HDM ChartCopilot™ Retro, we reduced chart review time by 40% and improved coding accuracy. Preparing RADV packets has never been easier."
— Medicare Advantage Plan Risk Adjustment Director
"The AI copilot flags missing documentation and guides coders in real time, saving countless hours."
— Senior Coding Auditor
"Analytics dashboards give us actionable insights into risk score gaps across multiple facilities."
— Health Plan Executive
FAQs
Q: Can HDM ChartCopilot™ Retro integrate with my EMR?
A: Yes, our solution supports most EMRs and claim systems, allowing direct chart imports.
Q: Is the AI making final coding decisions?
A: No, the AI assists your coders by highlighting potential HCCs and documentation, but final coding remains under human review.
Q: How secure is my data?
A: HDM ChartCopilot™ Retro is fully HIPAA-compliant, with end-to-end encryption and audit logs for all actions.
Q: How quickly can we see ROI?
A: Most clients report measurable productivity gains and coding accuracy improvements within the first 60 days of deployment.
Q: Can we customize workflows?
A: Yes, you can configure task sequences, alerts, and review processes to match your organizational needs.
Get Started Today
Accelerate retrospective chart coding, improve risk adjustment accuracy, and prepare RADV-ready charts efficiently.